Introduction: The Neck
Problems with the neck are very common, with pain and often limitation of movement that affects many everyday activities. Neck pain often spreads into the shoulder and neck problems can cause pins and needles and numbness in the hands. For this reason, it is often necessary to assess both the neck and the shoulder when dealing with a neck problem. However we shall consider the neck and shoulder separately, for simplicity.
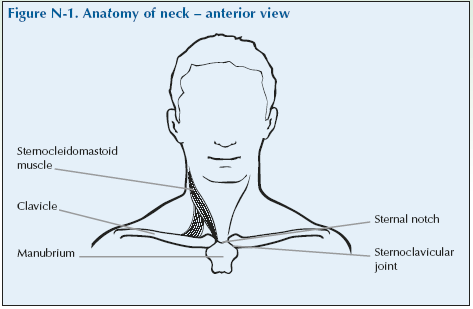
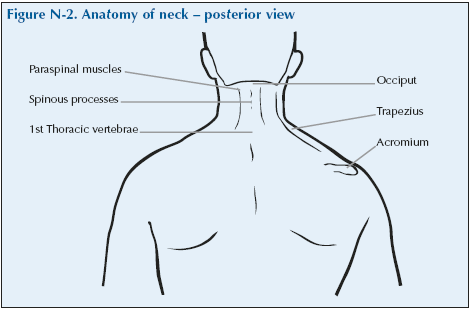
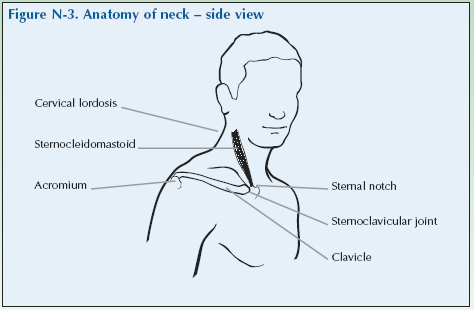
Anatomy of the Neck
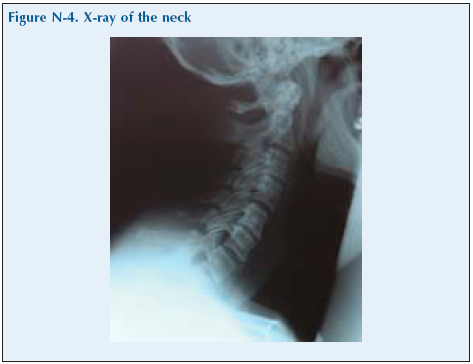
The neck is the upper part of the spine and is sometimes referred to as the cervical spine. The spinal column is comprised of a number of small bones or vertebrae (singular vertebra) separated by intervertebral discs. The cervical spine comprises seven vertebrae, which are numbered C1 to C7, starting at the skull and numbering towards the shoulder region. C1 is called the Atlas bone and C2 is the Axis. Each vertebra has a spinous process, which can easily be palpated in the midline posteriorly.
The nerves that supply the shoulders, arms and hands leave the spinal cord between the vertebrae of the neck. Therefore, problems with the vertebrae that cause pressure on, or trapping of, the nerve can be accompanied by pain or tingling in the shoulders, arms or fingers and, less commonly, may cause muscular weakness in the arms or hands, and rarely in the legs.
Neck Pain
The neck moves almost constantly during waking hours. Neck pain is common, over two thirds of the population experience some kind of neck pain that lasts for three or more months during their lives.
Neck problems can present with pain and stiffness in the neck and sometimes an accompanying headache. The pain can spread across to a shoulder and down the arm. These symptoms can be due to disorders in the neck itself or from the muscles going into spasm. Neck problems can also result in pins and needles in the hand and forearm if a nerve that is bringing sensation from the hand and forearm is pressed on or irritated as it passes through the forearm into the cervical spine.
Fig N-5
Neck pain may be due to:
[su_table]
| Cervical spondylosis with degeneration of the discs and osteoarthritis of the joints in the neck | Pain often spreads across into a shoulder and upper arm. May be associated with headache at the back of the head (often confused with migraine). Can be associated with irritation of the nerves to the arms with pins and needles in a hand as a result. Sometimes osteoarthritis of the joints can cause pressure on the nerves with tingling or pins and needles (parasthesiae) in the hand. If the pressure is more severe, there may be loss of feeling and of power. |
| Whiplash | Caused by a sudden jerking, for example the sudden stopping of a car, whiplash can result in acute neck pain with muscle spasm. It is self-limiting in most people but in a few it can take a long time to settle. |
| Poor posture or straining the neck | This often affects people in sedentary jobs that involve holding the neck in one position for long periods, for example looking at a computer screen. Also tasks which involve overhead work can provoke neck pain. |
| A prolapsed intervertebral disc | Prolapsed discs can cause pain that may spread down the back or arm. The disc may protrude into the spinal canal where it presses on nerves and can cause pain with tingling, loss of feeling and weakness. This is not very common in the neck and more often happens in the lower back. |
| Inflammatory arthritis including rheumatoid arthritis | The neck can be affected in ankylosing spondylitis and other similar types of arthritis with inflammation of the tissues around the joint. Rheumatoid arthritis can also affect the joints of the neck and can make the neck unstable (subluxation) – this is not seen so often now with the more effective treatment of RA. |
[/su_table]
Giving a History of Neck Problems
Invite the doctor to carry out a consultation by first asking you about your history related to the experience you have of your condition. This will then be followed by the physical examination.
The doctor should first ask you ‘What is the problem?’ and you should give a short response describing your symptoms and their effect on your quality of life.
Develop a script based on your own experience. You may still have the symptoms or you may be describing an episode you have had as if it were still present.
Describe as fully as you can your own symptoms, including where in the neck you feel/felt pain or discomfort and whether you have/had any tingling in your arms and/or hands. Say if you have any stiffness, swelling or other symptoms. Mention if you have/had any headaches and how the problem is having/had an impact on your daily life, your work or your sleep.
Remember to describe how your condition affects/affected your quality of life using the framework covered in the earlier section of this manual. Consider self care (e.g. ability to wash, dress, toilet and feed), domestic care (e.g. ability to cook, clean, launder, shop), work (e.g. ability to stand, sit, type), leisure (e.g. ability to play sports, walk, go out for meals). Explain about the way it limits/limited your activities and restricts/restricted your participation in normal life.
Do not tell him everything spontaneously – just the important part. He will then need to ask further questions to fully characterise your problem. Develop a set of answers with your trainer to the following points. Prompt them if they omit important questions.
Pain is usually present and questions should establish:
• How the pain started and developed.
• The nature of the pain.
• The exact distribution of the pain.
• Whether the pain has increased or decreased over time.
• Whether it affects sleep.
• Whether anything exacerbates or relieves the pain. Stiffness may be a symptom and questions should establish:
• If you are stiff at all?
• When it is worse?
• What improves it?
Swelling may be a symptom and questions should establish:
• If you have noticed any swelling and where.
• If it is always present.
• If it is painful or tender.
• If it is increasing.
They need to ask about the pattern of all the symptoms – where they started and if they have spread anywhere.
You may prompt the doctor (if you have not already told them) to make sure that they include the following information:
- Your hand dominance.
- Your age, occupation and hobbies.
- Whether you have injured or strained your neck.
- Your past medical history.
- Whether you have any symptoms such as tingling, numbness or weakness in your arms/hands/fingers.
- Whether there is any impairment of function and how this impacts on your daily activities and quality of life.
– Neck problems typically cause difficulty driving, reading, sleeping, looking up to change a light bulb, or performing any activity requiring the head to be held up or in the same position for a length of time. Working with the arms raised above shoulder height is often difficult as you look up to do this.
- Whether you have had previous treatment and if so whether it was successful.
The effect of any problem depends on your personal circumstances. The doctor needs to know about what you need to do in the home, at work, your leisure interests and your expectations.
You may have symptoms affecting other parts of your musculoskeletal system. You may prompt the doctor to ensure he has asked whether you have any other problems affecting your muscles, joints, neck or back.
You may go into further details about how your problem affects your life and the treatment you have received at the end of the session when discussing the findings.
Example of a Script
You should develop something like this, based on your own story. First you need to ask me:
“What is your problem?”
“I have had neck pain for several years which is worse when I wake up, and I also get pins and needles in my hands. It sometimes wakes me and I cannot do things that need me to look upwards for a long time.”
You should then respond to questions, guiding and prompting the doctor through the information as listed above.
Neck Examination Script
Describe the examination to the doctor using the anatomical and directional terms you have learnt. You can use your knowledge of anatomy best when the doctor is feeling the joint and periarticular structures.
“I would now like to invite you to find out a little bit more about my problems, by role play, using me as your patient and examining me.”
Examination of the cervical spine must be gentle, especially in those with severe rheumatoid arthritis. Some people with rheumatoid arthritis have an unstable spine because of joint damage and if the spine is forced to move beyond its limits neurological damage or subluxation of the cervical spine could occur. (Subluxation is partial dislocation of a joint so that the bones are still in contact but are not properly aligned).
Look
Inspect the patient’s posture and the alignment of the head and neck. The head and neck should be erect and perpendicular to the shoulders. Redness and swelling are rarely seen in the neck.
What do you see?
Feel
Feel for tenderness over the cervical spinous processes by palpating down the vertebrae using the index and/or middle fingers or thumbs. The patient may like to place their hands on a table or chair for support.
Feel for tenderness or spasm in the muscles approximately 1” (2.5cm) either side of the spinous processes. Move the flat surface of your finger tips in a circular motion and keep fingers in contact with the skin so as not to miss any findings.
What do you feel?
Move
Rotation: Evaluate rotation by asking the patient to sit facing you on the edge of the examining table or in a chair. Ask them to turn their head to the right as far as they can and estimate the angle. Repeat this to the left. Look for full or limited range of motion (ROM); remember flexibility diminishes with age.
Figure N-6. Rotation of neck
Lateral flexion: Lateral flexion can be assessed by asking the patient to angle their head to the right trying to touch their shoulder with their ear and then repeating this to the left. You may need to demonstrate the movement to them. Ask if this is the patient’s normal range of motion or whether they feel it is restricted.
Fig N-7
Flexion and extension: Assess flexion and extension by asking the patient to bend their head forward as far as they can. Then ask the patient to perform the reverse movement and to look up as far as possible. Estimate whether this is the full ROM or seems restricted; remember flexibility decreases with age. Ask the patient if the current range of motion is normal for them or if it has changed.
Fig N-8
What have you found?
Stress
It is very important that stress is never used when examining the neck.
Listen
Crepitus may be heard on movement. It tends to occur quite frequently in older people, even when they have no significant neck problem.
Special tests
As neck problems can be associated with irritation or pressure on the nerves to the arm, a neurological examination should also be done, especially if there are any symptoms of tingling, numbness or weakness in the arms or hands.
Lightly touch the arms and the palmar and dorsal surfaces of the hands and fingers and ask if sensation is normal. Test grip strength by asking them to wrap their fingers around two of yours and then to squeeze hard. Test pinch grip by asking them to pinch together their thumb and index finger hard and you seeing if you can break the circle. Tell them they should now test the reflexes in the arms (triceps, biceps and supinator jerks).
“We have now come to the end of this mock consultation. You should have learned quite a bit about my condition from taking my history and examining my joints, however, I would be happy to provide you with a bit more detail about the progress of my condition and how it affects my life, if you would find this useful.”
[Please give a brief description of your condition:
- When and how it started.
- Physical and psychological affects on you.
- Treatments offered.
- How your condition progressed.
- How this affected your life: Home, education, work, leisure, ability to travel, relationships etc.]
“Does anyone have any further questions?”
“Thank you again for attending this session. I hope you have found it useful.”